Highlights
- Canada lacks a consistent national approach to collecting and sharing critical health data.
- We do not have sufficient information about resource needs or who is best suited to provide care.
- This contributes to health inequalities, rising costs, pressure on the workforce and lack of accountability for health outcomes.
The AMC takes stock of…
According to a 2022 Commonwealth Fund survey, the Canadian health care system is ranks tenth place in the ranking of 11 high-income countries, ahead only of the United States. There are many ways to remedy this situation, but to choose the best solutions, you need to understand the gaps in the system.
Canada currently lacks a consistent national approach to collecting and sharing critical health data. We don’t have enough information about resource needs or who is best placed to provide care. Healthcare professionals and patients also suffer from a lack of interoperability between electronic health records. This contributes to health inequalities, rising costs, pressures on the workforce and a lack of accountability for health outcomes.
The Canadian Medical Association (CMA) is calling for urgent action to improve health data to modernize care, better manage workforce planning and enable more transparent tracking of outcomes.
“We cannot improve our health system without collecting and reporting data. The more information we have, the more accurately we can track our progress and ensure transparency.”
-DD Kathleen Ross, CMA President
What we don’t know
Organizations like CIHI provide important data. However, many questions remain unanswered and Canada’s many health authorities do not have a national database.
Here are some of the things we don’t know:
Where is the need for doctors and other health personnel greatest? What specializations are needed where?
Every health authority has information on staff shortages and waiting times, but we lack the overall picture to understand how to optimise resource allocation.
Are there overlaps between the fields of activity of the health professions?
It’s difficult to optimize the use of our healthcare professionals without data on their specific skills and how they can deliver more effective care as part of a team. For example, in 2023, pharmacy technicians in Ontario were allowed to prescribe medications for 13 minor conditions (such as dermatitis and uncomplicated urinary tract infections), leading to a reduction in the number of primary care physician consultations.
How many internationally trained physicians come to Canada to practice each year?
There is no national data to answer this question. The federal government recently announced funding for the Royal College of Physicians and Surgeons of Canada to help eligible applicants apply within three to four months of arrival, rather than the current six to twenty-four month wait. The Council of Canada wants to increase the use of fitness-to-practice assessments. However, there is no systematic collection of data on the entry of these physicians into practice.
How many doctors leave their profession every year?
Available indicators that determine when physicians retire from the profession include renunciation of licensure, cessation of provincial health insurance billing, and cessation of professional contributions. However, there is no national survey of the number of physicians retiring each year.
Is there comprehensive data on equity, diversity and inclusion in medicine?
Apart from gender, no.
How data can help – and save lives
Integrated workforce planning in healthcare
Currently, healthcare workforce planning is done in isolation and does not take into account changes in career longevity, demographics and the health needs of the population. To provide the right care in the right place and at the right time, we first need to have transparent and shareable data on the health workforce across all professions and regions combined, particularly with regard to planned retirements, turnover rates and training.
Population health management
Data helps health leaders understand the needs of patients today and tomorrow and allocate resources to prevent disease and optimize the care needed. In particular, it makes it possible to assess the social determinants of health, such as housing, food security and economic stability, as well as the aging of Canada’s population and understand which communities are at increased risk for certain diseases.
Empowering patients and healthcare providers
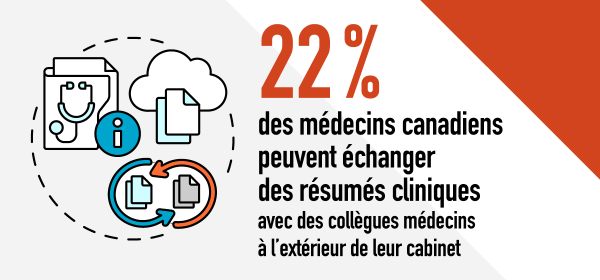
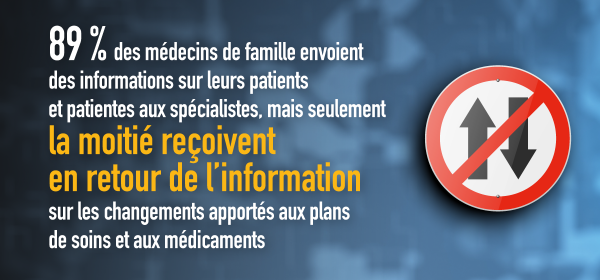
Access to personal health information (vaccination records and laboratory results) allows patients to manage their care more easily and helps establish a system that is more focused on partnership with patients. For healthcare providers, the ability to share information with colleagues in other healthcare professions and other regions is invaluable. This sharing makes it possible to reduce unnecessary examinations and gain a more comprehensive view of the patient situation.
COMPLETE CARE
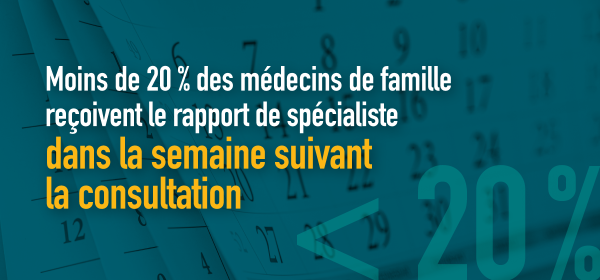
The lack of interoperability makes it difficult to exchange health data between doctors.
Sources: Results for Canada from the 2022 Commonwealth Fund (CMWF) International Health Policy Survey of Primary Care Physicians; Improving Accountability to Canadians in the Health Sector (CMA)
Future
Demands for improved health data are paying off.
The DR Alika Lafontaine, CMA President for 2022-2023, is part of the interim steering committee of Health Workforce Canada, a new organization created specifically to improve data collection.
This initiative is part of the Canadian government’s recent efforts to address the health data shortage. In 2023, the federal government announced five-year, $505 million in funding for the Canadian Institute for Health Information (CIHI), Canada Health Infoway and federal data partners. Specifically, these funds will be used to create a centre of excellence in health workforce data and planning and to improve access to and use of information in the care sector.
As part of the $46.2 billion increase in federal health funding over the next decade, provinces and territories must also commit to new ways of collecting, using and sharing data.
In the context of these historic funding arrangements, accountability is essential. A recent CMA report provides benchmarks for measuring health system performance and areas for improvement, including patient and physician access and data sharing.
What can doctors do to help?
To do better, we need to work with doctors and medical students of all ages and specialties, regardless of where they are in their careers or whether they work in rural and remote settings big cities.
Find out how you can contribute to the CMA’s efforts.
Learn more about CMA’s priority objectives

Award-winning entrepreneur. Baconaholic. Food advocate. Wannabe beer maven. Twitter ninja.